



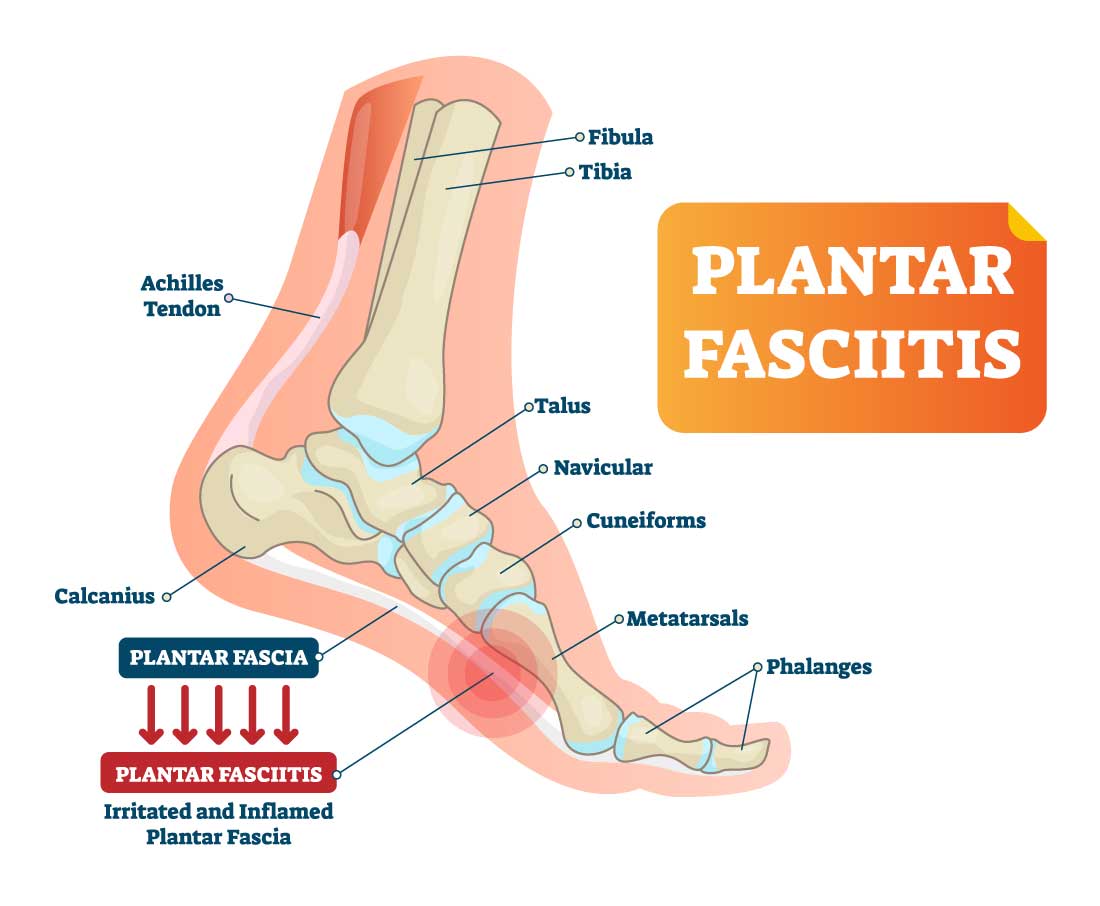
Plantar Fasciitis Explained
Plantar Fasciitis – (PLAN-tur fas-e-I-tis) is one of the most well-known reasons for heel and foot discomfort. It includes pain and inflammation of a thick band of tissue, called the plantar fascia, that runs from the heel to your toes on the sole of your foot.
Plantar fasciitis generally causes tremendous pain and is generally associated with your first morning steps, after sleeping. When your foot limbers up, after walking for a bit the torment of plantar fasciitis usually diminishes, however, it might return after significant stretches, standing, or subsequent to getting up from a rested position.

Who Are Typically At
Risk
In general some of these following factors can make you more inclined to develop plantar fasciitis. Individuals that become overweight, having fallen arches (flat feet) or high arches, over exercising, for example, significant distance running, dancing in high impact, occupations that require standing or walking on hard surfaces for extensive stretches of time and wearing shoes without appropriate arch support or worn out shoes.
Causes
Too much pressure over the fascia may damage or tear away the tissue and can be a cause of heel pain. It is also possible that when the plantar fascia gets overstretched or overused repeatedly, there may be irritation or inflammation of the fascia. Inflammation of the plantar fascia causes plantar fasciitis.
A lot of pressure and tension over the fascia might harm or tear away the tissue and can be a reason for heel pain. It is additionally conceivable that when the plantar fascia gets overextended or abused repeatedly, there might be inflammation or aggravation of the plantar fascia. Inflammation of the plantar fascia causes plantar fasciitis, and is considered the number one cause contributing to plantar fasciitis.


Symptoms or Alerts
The most well-known symptom of plantar fasciitis is the agonizing feeling as if someone is stabbing your foot in the heel area of the bottom of your feet. The pain and discomfort grow progressively and may include one or two feet simultaneously.
Pain is normally worse in the morning and subsequently can worsen as the day goes on, particularly after getting back on your feet after assuming a rested position at the beginning of the day or may bother subsequent to remaining standing for quite a while.
Podiatrist Recommended
Podiatrists and Orthopedists from around the country profoundly recommend Colony insoles™ as the 1st choice for an over-the-counter (OTC) Insole. Many Health care professionals select our Orthopedic Insole based on our quality and manufacturing techniques and overall performance. Colony Orthopedic insoles are rapidly becoming the #1 Insole sold in the USA.
The Dura-last foam used in our inserts is a closed-cell resin described by third parties as an injection-molded EVA foam. The EVA foam forms itself to the user’s feet and offers purported medical benefits, according to a number of Certified Podiatrists.
Diagnosing Plantar Fasciitis
Your treating physician will look at your foot and will check for the indications of flat feet or possibly high arches, redness, swelling, and tenderness of the foot. Also, your physician may examine the amount of flexion, extension, tightness, and stiffening of the arch on the sole of your foot.



Treatment – Most patients with plantar fasciitis are successfully treated with the accompanying measures listed below:
Prescriptions & Medications – Your treating physician might prescribe nonsteroidal mitigating drugs (NSAIDs) as they can lessen your pain and inflammation. Corticosteroids can be introduced by injecting them directly into the plantar fascia which might offer relief from discomfort and diminish inflammation.
Rest- Abatement or keep away from the exercises and activities that increase the pain.
Ice – Apply ice pack over the affected area two times per day for 10 – 15 minutes, for the first 3-5 days. Freezing a bottle of water and rolling your feet over the bottle is a very effective way to administer ice.
Night Supports – Utilization of night braces is helpful as it extends the plantar fascia and permits it to recuperate.
Supportive Shoes and Orthotics – Your primary care physician might suggest that you wear shoes with greater support and special cushioning. Custom orthotics (shoe insoles) may likewise be useful.
Physical Therapy (PT) – You may be suggested to enlist into a PT program that will concentrate on stretching the achilles tendon and the plantar fascia. These exercises may help to strengthen the muscles of the lower leg calf area. Additionally to those exercises, application of athletic taping to support the sole of your foot is also instructed.
Extracorporeal Shock Wave Therapy – This is a newer procedure to try and diminish and lessen the pain. During this procedure, sound waves are directed to the painful area to stimulate the healing process in the damaged plantar fascia tissue.
Surgery – Not often but and as a final if the previously mentioned approaches fail, surgery to release the tight plantar fascia may be needed. Again, it is recommended only after all nonsurgical measures have failed.
Preventive measures such as stretching exercise programs and footwear modifications can help prevent plantar fasciitis. But if it occurs proper treatment is essential as otherwise it can become a long-term problem.
